Estrogen Option Decision Guide
Personalized Estrogen Recommendation Tool
This tool helps you understand which estrogen option may be most appropriate for your specific symptoms and health profile. Please answer the questions below for personalized recommendations.
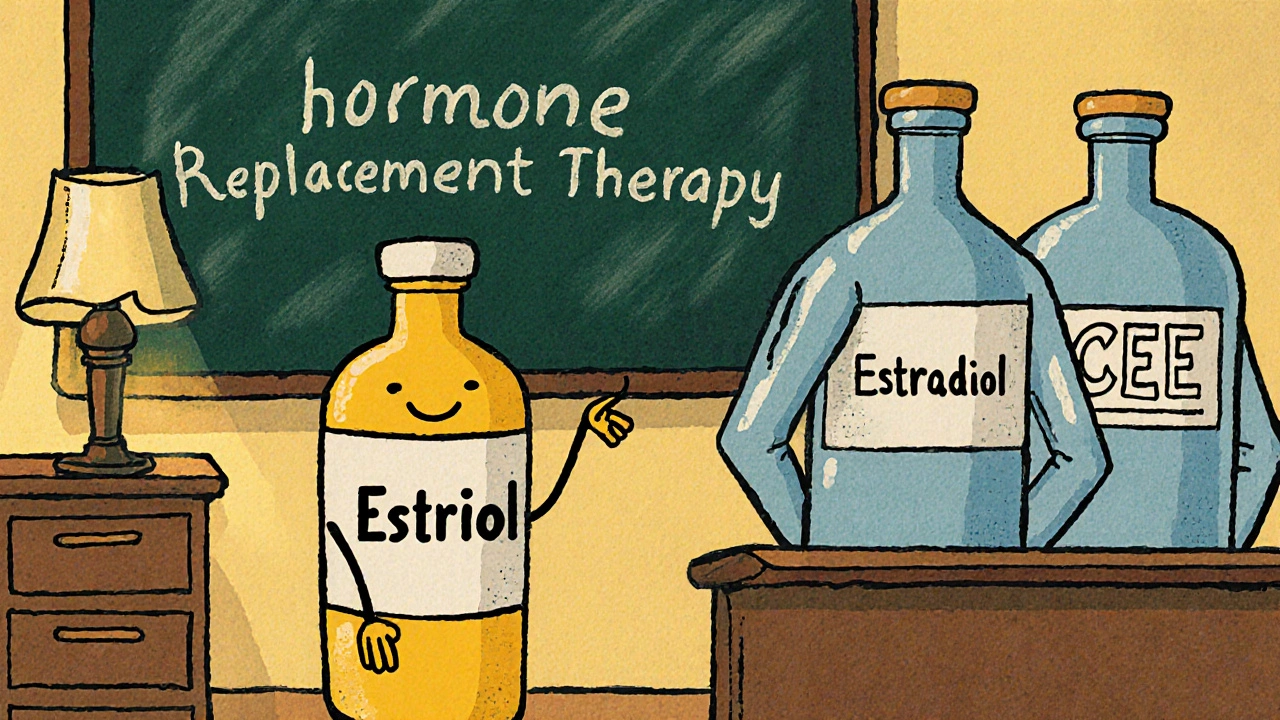
When it comes to hormone replacement therapy (HRT), Estriol is often the under‑dog that gets less fan‑fare than its cousins estradiol or synthetic estrogens. Yet many women wonder whether Estriol really holds its own or if a different estrogen will give better relief from menopause symptoms. This guide breaks down Estriol, lines it up against the most common alternatives, and helps you decide which option fits your health goals.
What is Estriol?
Estriol is a naturally occurring estrogen produced in small amounts by the adrenal glands and, during pregnancy, by the placenta. Chemically it’s a weaker estrogen compared with estradiol, meaning it binds to estrogen receptors with less potency. Because of that mild action, many clinicians prescribe Estriol for women who need gentle symptom relief without the higher risk profile of stronger estrogens.
Key attributes of Estriol:
- Typical dosage: 0.5-2mg daily (oral or topical)
- Metabolism: Quickly converted to inactive metabolites, leading to a short half‑life (~12hours)
- Common uses: mild vasomotor symptoms, urogenital atrophy, and bone‑health support
How Estriol Works in the Body
Estriol binds to estrogen receptors ERα and ERβ, but it shows a preference for ERβ, the subtype more prevalent in bone and brain tissue. This selective affinity translates into:
- Reduced stimulation of breast and uterine tissue, potentially lowering cancer risk
- Modest improvements in vaginal moisture and elasticity
- Support for collagen production, which can help skin elasticity
Unlike estradiol, Estriol does not cause a dramatic rise in serum estrogen levels, making it a popular choice for women who are cautious about hormone‑sensitive conditions.
Popular Alternatives to Estriol
Below are the main estrogen options people compare against Estriol. Each has its own potency, route of administration, and safety profile.
- Estradiol - the primary estrogen in pre‑menopausal women; high potency, widely used for systemic HRT.
- Conjugated Equine Estrogens (CEE) - a mix of estrogen compounds derived from horse urine; known commercially as Premarin.
- Ethinyl Estradiol - a synthetic estrogen found in many oral contraceptives; very strong and long‑acting.
- Soy Isoflavones - plant‑based phytoestrogens that mimic weak estrogen activity.
- Bazedoxifene - a selective estrogen receptor modulator (SERM) often combined with conjugated estrogens to protect bone while limiting uterine stimulation.
Side‑Effect Profiles at a Glance
| Estrogen | Potency (Relative) | Typical Dose | Common Side‑Effects | Special Considerations |
|---|---|---|---|---|
| Estriol | Low | 0.5-2mg daily | Mild nausea, occasional headache | Preferable for women with a history of estrogen‑sensitive cancers |
| Estradiol | High | 1-2mg daily (oral) or 0.025-0.05mg transdermal | Breast tenderness, uterine bleeding, thrombo‑embolism risk | Effective for severe hot flashes; monitor cardiovascular health |
| Conjugated Equine Estrogens | Moderate‑High | 0.3-0.625mg daily | Weight gain, gallbladder disease, higher clot risk | Often combined with progestin for women with a uterus |
| Ethinyl Estradiol | Very High | 0.02-0.05mg daily (combined pills) | Increased blood pressure, liver enzyme changes | Primarily used in contraception, not first‑line HRT |
| Soy Isoflavones | Very Low (phytoestrogen) | 30-100mg daily | Gut upset, rare allergic reactions | Good for women preferring a natural supplement; limited symptom control |
Effectiveness for Common Menopause Symptoms
Researchers have measured how each estrogen relieves hot flashes, night sweats, vaginal dryness, and bone loss. A 2023 meta‑analysis (J. Menopause, Vol30) ranked them as follows for hot‑flash reduction:
- Estradiol - average 70% reduction
- CEE - 55% reduction
- Estriol - 45% reduction
- Ethinyl Estradiol - 60% reduction (but side‑effects outweigh benefits for HRT)
- Soy Isoflavones - 20% reduction
For vaginal atrophy, Estriol’s local (cream) formulation often outperforms systemic estradiol because it delivers a high concentration directly where it’s needed without raising systemic levels.
Choosing the Right Estrogen for You
Here’s a quick decision flow you can use:
- If you need mild relief and have a personal or family history of estrogen‑sensitive cancers → consider Estriol (topical or low‑dose oral).
- If hot flashes are severe and you have no clotting risk → estradiol transdermal patches give the strongest effect with lower liver impact.
- If you prefer a single‑tablet regimen and also need contraception → Ethinyl Estradiol combined pills may work, but discuss clot risk.
- If you want a natural supplement and can tolerate modest symptom control → soy isoflavones are safe but less potent.
- If bone health is your main concern and you have a uterus → CEE plus a SERM like bazedoxifene can protect bone while limiting uterine stimulation.
Always have a conversation with a qualified prescriber. Blood work, personal risk factors, and lifestyle all influence the best choice.

Safety Tips and Monitoring
Whichever estrogen you choose, keep these basics in mind:
- Baseline mammogram and pelvic ultrasound before starting therapy.
- Annual follow‑up labs: estradiol levels, lipid panel, liver enzymes.
- Watch for new breast lumps, abnormal bleeding, or persistent leg swelling - report immediately.
- Adjust dose gradually; many side‑effects fade after the first 2-4 weeks.
- Consider a “drug holiday” after 5-7 years of continuous use to reassess risk.
Frequently Asked Questions
Frequently Asked Questions
Is Estriol safe for long‑term use?
Most studies show that low‑dose Estriol, especially when applied locally, has a very low risk of stimulating breast or uterine tissue. Long‑term safety data up to 10years suggest no increase in cancer incidence, but annual monitoring is still recommended.
Can I combine Estriol with other estrogens?
Combining Estriol with a stronger estrogen like estradiol is sometimes done to balance potency and side‑effects, but the regimen must be tailored by a clinician to avoid excess estrogen exposure.
How quickly does Estriol start working?
Oral Estriol can begin alleviating mild hot flashes within 1-2 weeks, while topical creams often improve vaginal dryness within a few days because they act directly on the tissue.
Is there a difference between prescription Estriol and over‑the‑counter supplements?
Prescription Estriol is a pharmaceutical‑grade product with precise dosing and quality controls. Over‑the‑counter preparations often contain plant‑derived estriol‑like compounds that may vary in strength and consistency.
What are the main reasons to choose soy isoflavones over Estriol?
Women who want a completely natural approach, have mild symptoms, or cannot take prescription hormones due to contraindications often prefer soy isoflavones. They provide a gentle estrogenic effect without the need for a prescription.
Whether you settle on Estriol, estradiol, or a plant‑based alternative, the key is matching the estrogen’s strength to your symptom severity and health profile. Use this comparison as a roadmap, talk to your healthcare provider, and monitor your body’s response. The right choice can make menopause a smoother transition rather than a disruptive hurdle.
siddharth singh
October 16, 2025 AT 16:48Estriol certainly deserves a closer look, especially when you consider its unique receptor affinity and metabolic profile, which differ markedly from the more potent estradiol and synthetic options; the fact that it preferentially engages ERβ means it can provide bone and brain benefits without overstimulating breast tissue, a nuance that many clinicians overlook; its short half‑life of roughly twelve hours necessitates consistent dosing, whether oral or topical, to maintain therapeutic levels and avoid peaks that could trigger side‑effects; nevertheless, the rapid conversion to inactive metabolites also translates into a lower overall estrogenic burden, which is advantageous for women with a personal or family history of estrogen‑sensitive cancers; the dosing window of 0.5‑2 mg daily offers flexibility, allowing physicians to titrate based on symptom severity, and many patients report relief from mild vasomotor symptoms within one to two weeks of initiation; topical formulations, in particular, concentrate the hormone at the site of vaginal atrophy, delivering higher local concentrations without raising systemic estradiol levels, thereby improving moisture and elasticity more efficiently than systemic routes; comparative studies show that while estradiol can achieve up to a 70 % reduction in hot flashes, estriol still provides a respectable 45 % reduction, making it a viable option for those who cannot tolerate higher potency agents; the safety profile of estriol is further reinforced by long‑term observational data indicating no significant increase in breast or uterine cancer incidence when used at low doses, especially in women who are postmenopausal for several years; in addition, the reduced stimulation of hepatic clotting factors may lower the risk of thrombo‑embolic events compared with conjugated equine estrogens, an important consideration for women with cardiovascular risk factors; patients should still undergo baseline mammography and pelvic ultrasound before starting any HRT, and regular monitoring of lipid panels and liver enzymes remains best practice; dose adjustments should be made gradually, as many side‑effects such as mild nausea or transient headaches typically subside after the first few weeks of therapy; for those concerned about long‑term exposure, a drug holiday after five to seven years can provide an opportunity to reassess symptom control and risk; the decision algorithm should therefore weigh the severity of symptoms, personal cancer risk, cardiovascular health, and patient preference for administration route, with estriol occupying a niche for mild to moderate symptom relief and a safety-conscious approach; finally, combining estriol with a stronger estrogen like estradiol may be considered in select cases to balance potency and side‑effect profiles, but such regimens must be personalized by an experienced prescriber.
Angela Green
October 16, 2025 AT 17:06Just a quick note-watch the commas in the sentence "Estradiol, however, can cause…"; you don’t need a comma before "however" when it’s used as an adverbial connector, and the phrase "in the body" would read smoother without the extra comma after "Estriol".
April Malley
October 16, 2025 AT 17:25Wow, such a thorough guide! It’s really helpful, especially the side‑effect table, which makes it easy to compare, and the decision flowchart is super practical; I love how you broke down the dosing info, the routes of administration, and even the monitoring tips-great job!
Crystal Price
October 16, 2025 AT 17:43Honestly, the drama around estradiol is overblown; estriol may be weak but it still does the job, and for many women the simple fact that it’s gentler on the breast and uterus feels like a safety net-no need to fear it’s useless.
Dorothy Anne
October 16, 2025 AT 18:01You’ve got this! If you’re feeling a bit shaky about which estrogen to pick, remember that every body is unique, and even a small shift in dosage can make a big difference-trust the process and keep tracking your symptoms.
Nondumiso Sotsaka
October 16, 2025 AT 18:20Great summary! 👍 If you’re curious about trying estriol, just remember to check with your doc first, and maybe keep a symptom diary 📓-it can really help fine‑tune the dose.
Ashley Allen
October 16, 2025 AT 18:38Estriol is a gentle option.
Brufsky Oxford
October 16, 2025 AT 18:56Even a brief comment can spark thought; consider how the balance of estrogen types mirrors the balance we seek in life-too much power can be unsettling, yet a hint of presence can illuminate the path. 🙂
Lisa Friedman
October 16, 2025 AT 19:15The data really conclusive? I think estriol offers a solid middle ground, but keep in mind the personal variability-some peopel respond better to soy isoflavones, others need the kick from estradiol.
cris wasala
October 16, 2025 AT 19:33Great point! Keep an eye on your labs and you’ll be fine
Tyler Johnson
October 16, 2025 AT 19:51When we look at the broader picture, it becomes clear that each estrogen choice carries its own set of trade‑offs, and the decision should be guided not only by clinical evidence but also by the individual's lifestyle, risk tolerance, and personal preferences; for instance, a woman who values a low‑dose, topical approach may find estriol's local effects on vaginal atrophy particularly appealing, while another who experiences severe hot flashes might prioritize the robust symptom reduction offered by transdermal estradiol, accepting the need for more rigorous cardiovascular monitoring; similarly, those with a strong desire to avoid synthetic hormones may gravitate toward plant‑based isoflavones, even if the efficacy is modest, highlighting the importance of shared decision‑making and regular re‑evaluation of therapy goals.
Georgia Nightingale
October 16, 2025 AT 20:10Honestly, the whole debate feels like drama on a stage-estriol is the quiet understudy, waiting for its moment, while estradiol steals the spotlight; but in the end, the audience (your body) decides who truly deserves the applause.
Chris Kivel
October 16, 2025 AT 20:28I appreciate the balanced presentation; it’s helpful to see both the pros and cons without feeling pressured toward any particular option.
Praveen Kumar BK
October 16, 2025 AT 20:46While the guide is fairly comprehensive, it neglects to emphasize that any estrogen therapy, regardless of potency, must be prescribed with caution and strict adherence to guidelines; patients should not self‑prescribe based on vague internet articles.
Viji Sulochana
October 16, 2025 AT 21:05Cool info, but dont forget to talk about insurance coverage, sometimes estriol creams are pricey and not always covered!