Unstable Angina: What It Is, How to Spot It, and What to Do
If you’ve ever felt a tightness in your chest that comes and goes, you might think it’s just stress. But when that pressure shows up unexpectedly, lasts longer than a few minutes, or gets worse with activity, it could be unstable angina – a warning sign that the heart isn’t getting enough blood.
Unstable angina is different from the occasional chest ache most people get after climbing stairs. It’s more serious because the blockage in the coronary artery can change quickly, raising the risk of a full‑blown heart attack. The key thing to remember: it’s a medical emergency that needs prompt attention.
Typical Symptoms You Shouldn't Ignore
The pain or discomfort usually sits behind the breastbone, but it can travel to the jaw, neck, shoulder, back, or even the arm. Many describe it as a pressure, squeezing, or burning feeling. Unlike stable angina, which eases with rest, unstable angina may linger for 10 minutes or more and won’t always disappear after you stop moving.
Other clues include shortness of breath, nausea, cold sweats, or an uneasy feeling in the stomach. Some people experience these signs while they’re at rest, especially during the night. If any of these pop up suddenly, treat them as a red flag and call emergency services right away.Women often have subtler symptoms such as fatigue, light‑headedness, or vague discomfort. Don’t brush those off – they can still point to unstable angina.
Why It Happens and Who’s at Risk
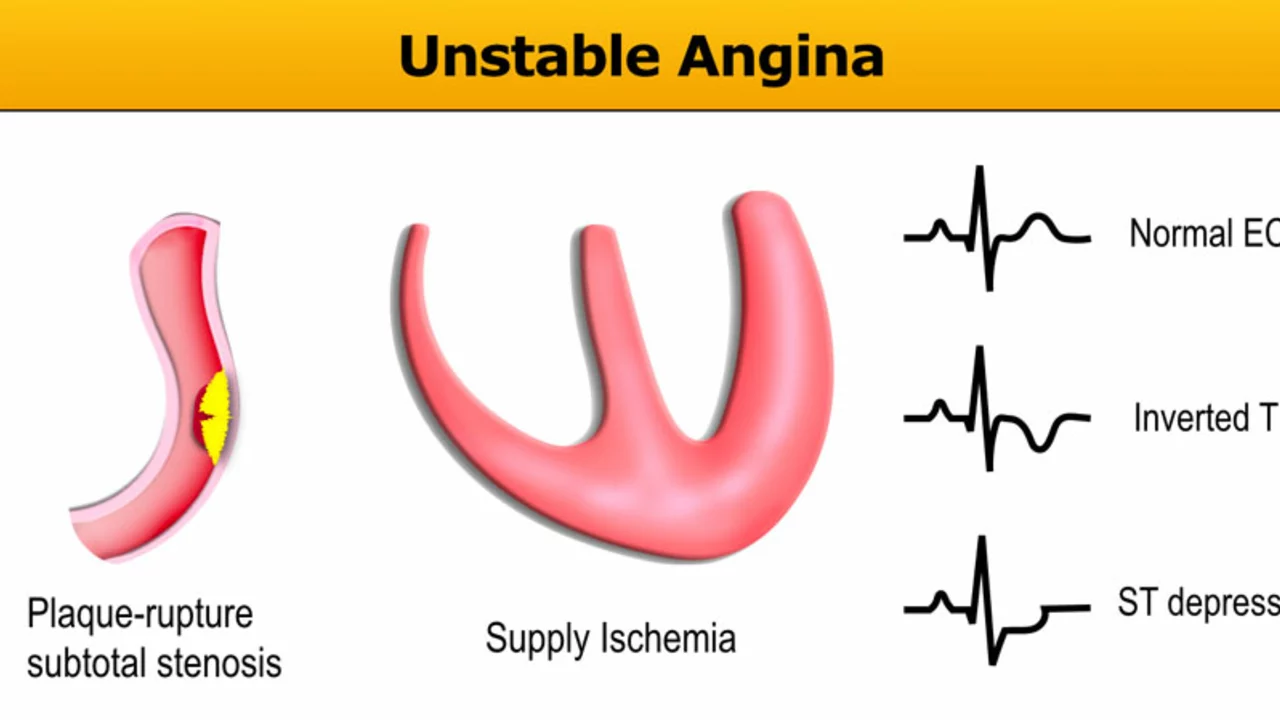
The main culprit is a build‑up of plaque in the coronary arteries. When a piece of that plaque ruptures or a clot forms, it narrows the artery just enough to cut blood flow but not completely block it. This creates an unstable situation where the heart muscle can start hurting even with light activity.
Risk factors include smoking, high cholesterol, high blood pressure, diabetes, obesity, and a family history of heart disease. Age matters too – men over 45 and women over 55 are more likely to develop it. If you have any of these risk factors, keep a close eye on your chest health.
Doctors confirm unstable angina with an electrocardiogram (ECG) and blood tests that look for heart‑damage markers. Sometimes they’ll do a stress test or a coronary angiography to see exactly where the blockage is.
Quick Actions and Treatment Options
The first step is to get to an emergency department fast. While waiting for help, chew an aspirin if you’re not allergic – it can thin your blood and limit clot growth. Nitroglycerin tablets or spray can also ease the chest pain, but only use them as directed by a doctor.
In the hospital, doctors may give you additional anti‑platelet drugs (like clopidogrel), blood thinners, beta‑blockers, or statins to stabilize the plaque. If the blockage is severe, they might perform angioplasty – threading a tiny balloon into the artery and inflating it to open the passage, often followed by placing a stent.
Long‑term care means lifestyle changes: quit smoking, adopt a heart‑healthy diet (think lots of veggies, lean proteins, whole grains), stay active with moderate exercise, and keep blood pressure and cholesterol in check. Regular follow‑up appointments let your doctor adjust meds and monitor progress.
Unstable angina is a clear signal that the heart needs help now, not later. Recognizing the symptoms, acting fast, and following up with proper treatment can prevent a heart attack and keep you on the road to recovery.
In my latest blog post, I delve into the heart condition known as unstable angina, explaining what it is, how it manifests, and why it's important to seek immediate medical attention when symptoms occur. We also discuss the various risk factors and the crucial role of lifestyle changes in managing this condition. I've included expert advice on treatment options, such as medication, angioplasty, and coronary artery bypass surgery. You'll also find tips on how to minimize the risk of unstable angina through regular exercise, a healthy diet, and stress management. Remember, early detection and management are key to living a healthy life with this condition.
Read More