When you take a medication, you expect relief - not a life-threatening reaction. But sometimes, even common drugs can trigger a severe adverse drug reaction that turns routine care into a medical emergency. These reactions don’t wait for a doctor’s appointment. They strike fast, and the difference between acting quickly and delaying can mean the difference between life and death.
What Counts as a Severe Adverse Drug Reaction?
A severe adverse drug reaction isn’t just a rash or an upset stomach. It’s a dangerous, unexpected response that threatens your life or causes permanent harm. The U.S. Food and Drug Administration defines it as any reaction that leads to death, is life-threatening, requires hospitalization, causes disability, or damages a major organ. The World Health Organization says it’s any harmful, unintended effect from a drug taken at normal doses.Some reactions happen within minutes. Others creep in over days or weeks. But when they turn severe, they all demand the same thing: immediate action.
Signs You Need Emergency Care Right Now
Not every side effect is an emergency. But these symptoms are red flags:- Sudden swelling of the lips, tongue, throat, or face
- Difficulty breathing, wheezing, or feeling like your airway is closing
- Dizziness, fainting, or a sudden drop in blood pressure
- Rapid heartbeat or cold, clammy skin
- A spreading rash with blisters, peeling skin, or raw, painful areas
- High fever with rash and swollen lymph nodes
- Dark urine, yellowing skin, or severe abdominal pain
If you or someone else shows even one of these after taking a new medication - call emergency services. Don’t wait. Don’t text a friend. Don’t check Google. Emergency means now.
Anaphylaxis: The Fastest Killer
The most dangerous reaction is anaphylaxis. It’s an all-out immune system meltdown triggered by drugs like antibiotics, NSAIDs, or even contrast dye used in imaging scans. It can start in under five minutes.Symptoms include:
- Hives or flushing
- Swelling in the throat that makes swallowing or breathing hard
- Wheezing or gasping for air
- Weak pulse, confusion, or loss of consciousness
Untreated, anaphylaxis kills 0.3% to 1% of people. But with prompt treatment, survival rates jump to over 99%. The key is epinephrine - and it must be given fast.
Epinephrine auto-injectors (like EpiPens) are the first-line treatment. Inject into the outer thigh. Even if you’re not sure it’s anaphylaxis, give it. Delaying epinephrine is the most common reason people die from this reaction. The Resuscitation Council UK says: “Initial treatment should not be delayed by a lack of a complete history or definite diagnosis.”
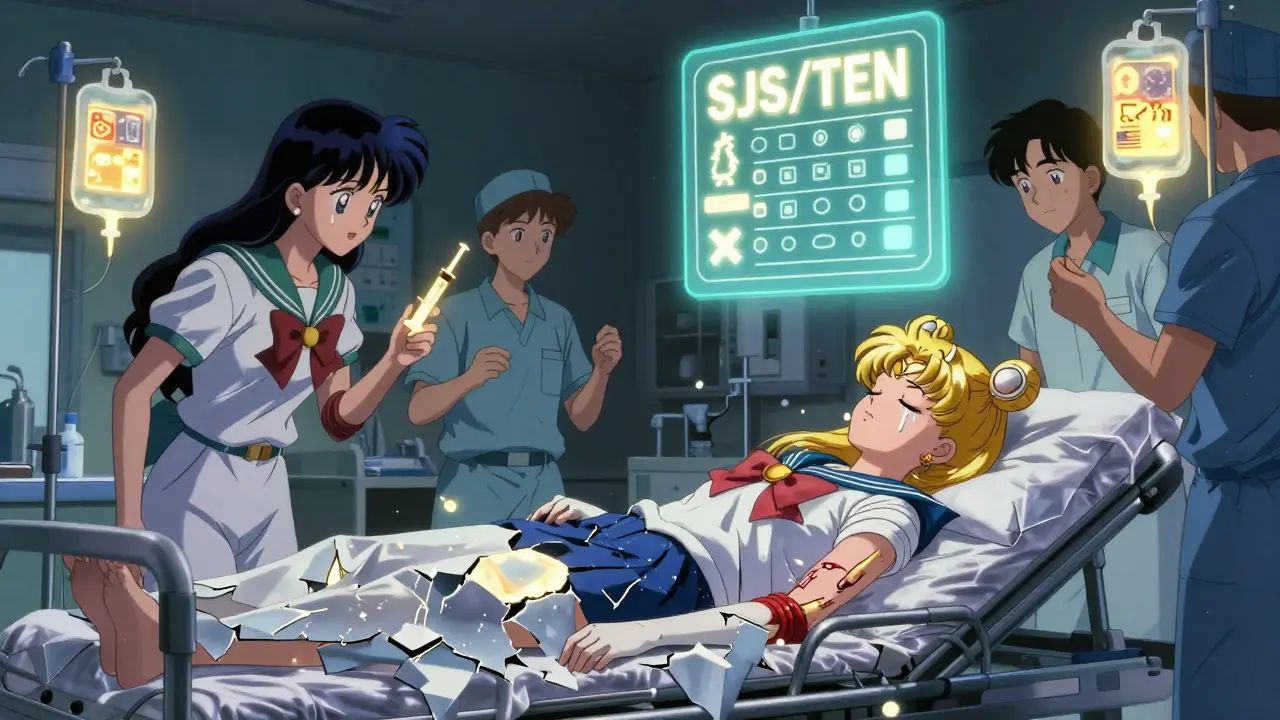
Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: Skin That Starts to Die
These are rare but devastating. They often start like the flu - fever, sore throat, burning eyes - then turn into a painful, spreading rash. Blisters form. Skin begins to peel off in sheets, like a severe burn.It’s usually caused by drugs like sulfa antibiotics, seizure meds (like carbamazepine), or painkillers (like ibuprofen or naproxen). The condition is called Stevens-Johnson Syndrome (SJS) if less than 10% of your skin detaches. If more than 30% peels off, it’s Toxic Epidermal Necrolysis (TEN). TEN has a 30% to 50% death rate.
There’s no home fix. You need a hospital - often a burn unit. Stopping the drug immediately is critical. Steroids and IV immunoglobulins may help, but recovery takes weeks. Survivors often lose vision, have chronic pain, or suffer scarring.
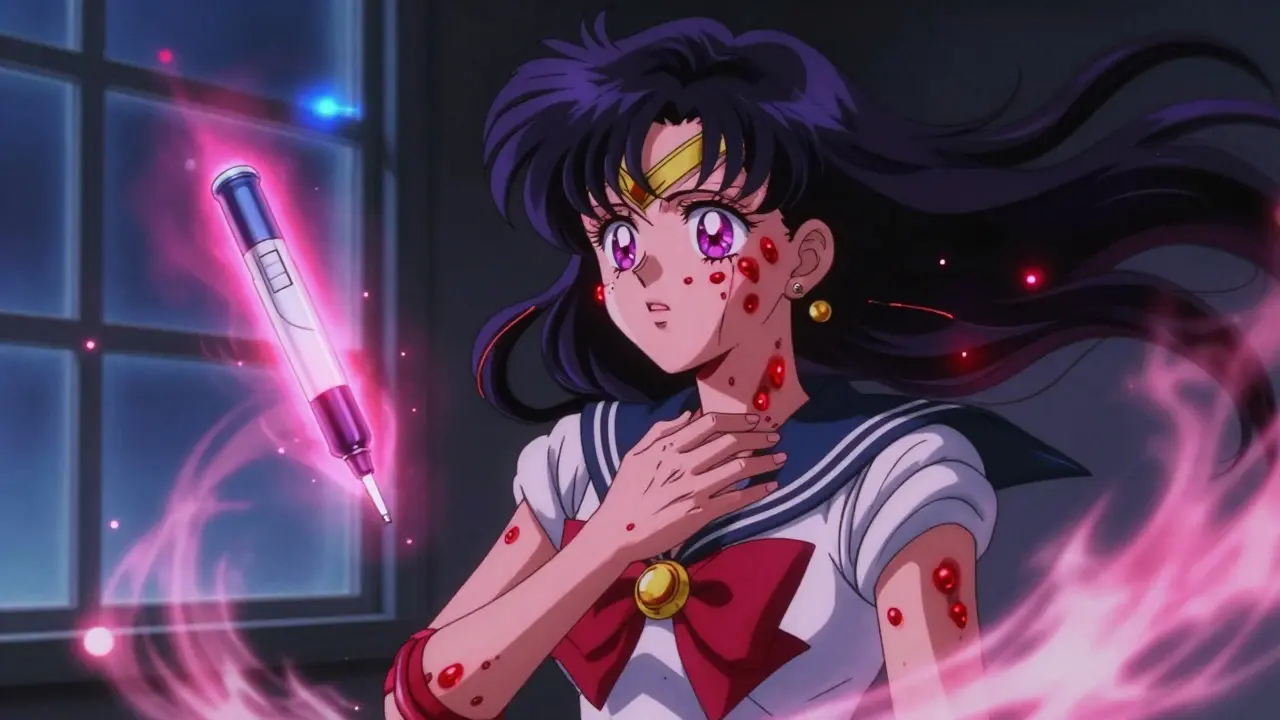
DRESS Syndrome: The Slow-Motion Crisis
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) doesn’t hit fast. It shows up 2 to 6 weeks after starting a drug. That’s why people miss the link.Symptoms include:
- Fever over 38°C (100.4°F)
- Widespread rash
- Swollen lymph nodes
- Liver or kidney damage
- Elevated white blood cells, especially eosinophils
Common culprits: anticonvulsants, allopurinol, and some antibiotics. It can destroy your liver or kidneys. If you’ve been on a new drug for a few weeks and suddenly feel awful with a rash and fever - get checked. Delayed treatment raises the risk of organ failure.
What to Do If You Suspect a Severe Reaction
1. Stop the drug immediately. Don’t wait to talk to your doctor. If you’re having trouble breathing or swelling - stop taking it right now. 2. Call emergency services. Don’t drive yourself. Don’t wait for a ride. Dial the local emergency number. Paramedics carry epinephrine and can start treatment en route. 3. Use your epinephrine auto-injector if you have one. Inject into the outer thigh. Hold for 3 seconds. Even if symptoms improve, you still need to go to the hospital. A second wave can hit hours later. 4. Bring your medication list. When you get to the ER, bring all your pills, bottles, or a list with names and doses. This helps doctors spot the culprit fast. 5. Don’t take the drug again. Once you’ve had a severe reaction, re-exposure can be fatal. Tell every doctor, dentist, and pharmacist from now on.Who Should Carry an Epinephrine Auto-Injector?
If you’ve ever had a severe allergic reaction to a drug - especially anaphylaxis - you should carry an epinephrine auto-injector. The American Academy of Family Physicians recommends it for anyone with a history of IgE-mediated drug reactions.Train everyone in your household how to use it. Practice with a trainer device. Keep one at home, one at work, and one in your bag. Expired injectors still work in an emergency - better than nothing.

How to Prevent Future Reactions
- Know your triggers. If you reacted to penicillin, avoid all penicillin-class drugs. Cross-reactivity is real. - Wear a medical alert bracelet. It tells first responders your allergies before you can speak. - Ask about alternatives. If you’re allergic to one painkiller, there are others. Don’t assume all NSAIDs are the same. - Report reactions. Tell your doctor and file a report with your country’s drug safety agency. This helps protect others.Over 20 million suspected drug reactions are reported worldwide each year. Most are mild. But the ones that turn deadly? They’re often preventable - if we act fast.
What Happens After the Emergency?
After surviving a severe reaction, you’ll likely be referred to an allergy specialist. They’ll do tests - skin prick tests, blood tests, or controlled drug challenges - to confirm what caused it.You’ll get a written emergency plan. This includes:
- Exact drug names to avoid
- Safe alternatives
- When and how to use your epinephrine
- Who to contact in an emergency
Some people need lifelong avoidance. Others can safely take the drug again under strict medical supervision - but only after testing.
The goal isn’t fear. It’s awareness. You don’t need to avoid all meds. You just need to know which ones could hurt you - and how to respond before it’s too late.
Can a mild drug reaction turn severe later?
Yes. A rash or itching after taking a drug might seem minor at first, but it can be the early sign of a severe reaction like DRESS or Stevens-Johnson Syndrome. These can develop over days or weeks. If a mild reaction gets worse - or if you develop fever, swelling, or trouble breathing - seek help immediately.
Can I take a drug I had a reaction to if it’s been years?
Never assume you’re safe just because it’s been a long time. Drug allergies can last a lifetime. Re-exposure can trigger an even worse reaction. Always tell your doctor about past reactions. They may refer you to an allergist for testing before considering rechallenge.
Do all antibiotics cause severe reactions?
No. But certain ones are more likely. Penicillins, sulfonamides, and cephalosporins carry higher risks of allergic reactions. Other antibiotics like azithromycin or doxycycline are less likely to trigger severe reactions. Your doctor can help choose safer options based on your history.
Is it safe to use someone else’s epinephrine auto-injector?
Yes. In a life-threatening emergency, using someone else’s epinephrine is better than doing nothing. The dose is standardized. Even if it’s expired, it’s still better than no treatment. Save a life - then call for help.
Can I get tested to find out what drugs I’m allergic to?
Yes. Allergists can perform skin tests or blood tests for certain drugs, especially penicillin. For others, a controlled drug challenge - done in a hospital with emergency support - may be needed. Testing helps you avoid unnecessary drug avoidance and find safe alternatives.
Are over-the-counter painkillers safe if I’ve had a reaction before?
Not necessarily. If you had a severe reaction to ibuprofen or naproxen, you may also react to other NSAIDs. Acetaminophen (paracetamol) is often a safer choice, but it’s not risk-free. Always check with your doctor before switching painkillers.
What if I don’t know what drug caused the reaction?
Tell the ER team everything you’ve taken in the last 2 weeks - including supplements, herbal products, and new prescriptions. Doctors use timelines and patterns to identify likely culprits. Even if you’re unsure, stopping all new medications until you’re evaluated is the safest move.
What Comes Next
If you’ve survived a severe reaction, your life changes. You’ll need to be more careful. But you don’t need to live in fear. With the right knowledge, tools, and communication, you can manage your risks and stay safe.Keep your emergency plan handy. Teach your family how to use epinephrine. Talk to your pharmacist every time you get a new prescription. And never ignore a symptom that feels wrong - because sometimes, the body’s warning comes before the diagnosis.
dean du plessis
December 27, 2025 AT 20:23Liz MENDOZA
December 28, 2025 AT 09:45Kylie Robson
December 28, 2025 AT 13:54Paula Alencar
December 29, 2025 AT 01:04Nikki Thames
December 29, 2025 AT 16:15Chris Garcia
December 30, 2025 AT 05:23Kishor Raibole
December 31, 2025 AT 11:53John Barron
January 1, 2026 AT 15:00Nicola George
January 3, 2026 AT 01:33Jane Lucas
January 3, 2026 AT 02:17Olivia Goolsby
January 3, 2026 AT 14:54James Bowers
January 4, 2026 AT 10:14