What Is Retinal Vein Occlusion?
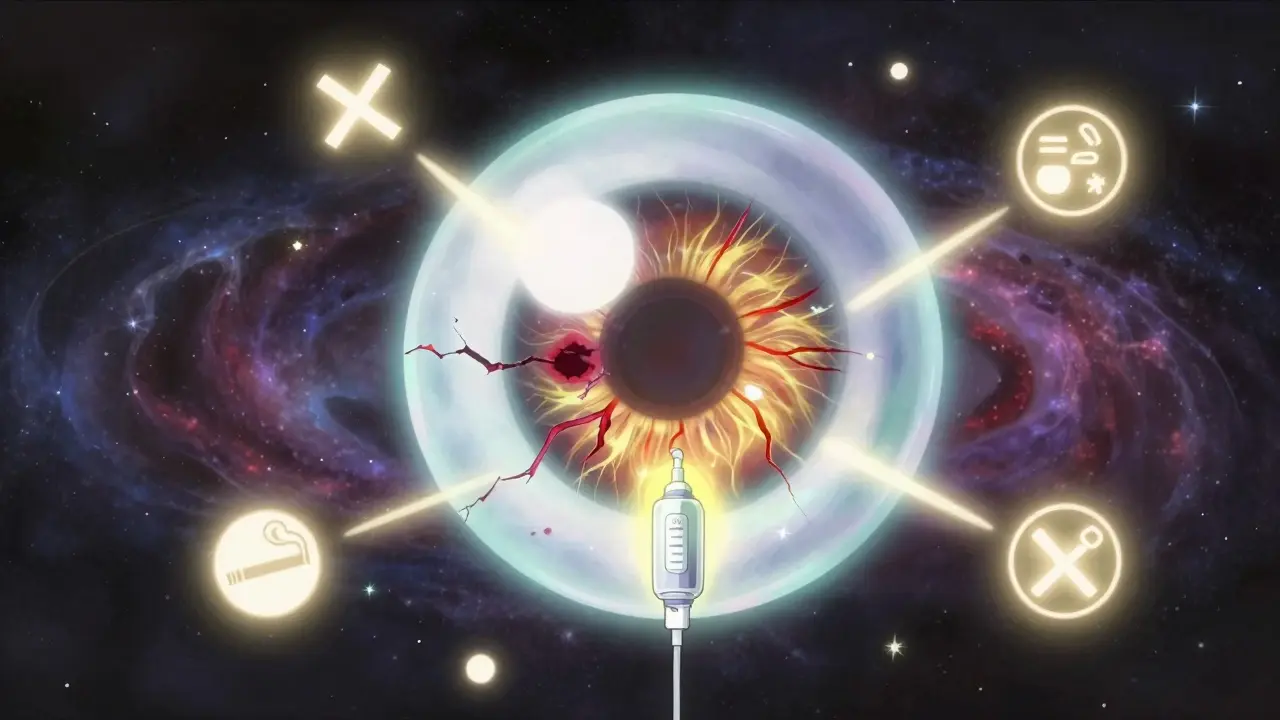
Retinal vein occlusion (RVO) happens when a vein in the retina gets blocked, stopping blood from flowing out. This causes fluid to leak, swelling the macula - the part of the eye responsible for sharp, central vision. The result? Sudden, painless blurring or loss of vision in one eye. It’s not a slow, creeping problem. Most people notice it all at once - like a curtain falling over part of their sight.
There are two main types: central retinal vein occlusion (CRVO), which blocks the main vein, and branch retinal vein occlusion (BRVO), which affects smaller branches. BRVO is more common and often happens where a hardened artery crosses over a vein and squeezes it shut. CRVO tends to be more severe and affects vision more dramatically.
It’s not rare. Around 16.4 million people worldwide have had RVO, and it’s one of the top causes of vision loss in people over 50. The good news? Treatment has improved dramatically in the last decade. The bad news? It’s not something you can just wait out. Left untreated, permanent damage can happen.
Who’s Most at Risk?
Age is the biggest risk factor. Over 90% of CRVO cases happen in people over 55, and more than half of all RVO cases occur after age 65. But it’s not just an older person’s disease - about 5 to 10% of cases strike people under 45. That’s why younger adults shouldn’t ignore sudden vision changes.
High blood pressure is the #1 risk factor. Up to 73% of CRVO patients over 50 have it. Even if you think your blood pressure is "controlled," if it’s not perfectly managed, you’re still at risk. Diabetes is another major player - about 10% of RVO patients over 50 have it, and it makes recovery harder. High cholesterol? That’s a factor in 35% of cases, no matter your age.
Glaucoma raises the risk too, especially when pressure builds up at the edge of the optic nerve. Smoking increases your chances by 25-30%. Being overweight or inactive adds to the pile. Hardened arteries (atherosclerosis) are the root cause in most cases - the same process that leads to heart attacks and strokes.
For younger women under 45, birth control pills are a known trigger, especially for CRVO. If you’re on the pill and suddenly lose vision, get checked immediately. Blood disorders like polycythemia vera, leukemia, or inherited clotting problems (like factor V Leiden) can also cause RVO in younger people. These are rare, but they’re important to rule out.
How Do Injections Help?
Injections don’t fix the blocked vein. They fix what happens after - the swelling in the macula called macular edema. That swelling is what blurs your vision. The goal of treatment isn’t to unblock the vein - it’s to stop the damage it causes.
Two types of injections are used: anti-VEGF drugs and corticosteroids.
Anti-VEGF injections - like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) - block a protein that causes blood vessels to leak. These are the first-line treatment. In clinical trials, patients gained 16-18 letters on the eye chart after 6 months. That’s like going from 20/200 (legally blind) to 20/60 - enough to drive in many places.
Corticosteroid injections, like Ozurdex (dexamethasone implant), reduce inflammation. They’re used when anti-VEGF doesn’t work well enough, or for patients who can’t handle frequent shots. One study showed 27.7% of CRVO patients gained 15+ letters with Ozurdex, compared to 12.9% with a placebo.
Bevacizumab (Avastin) is used off-label and costs about $50 per shot, while Lucentis and Eylea cost nearly $2,000. Many safety-net clinics use Avastin because it’s just as effective for many people. But in private practices, the more expensive options are more common.
What Does Treatment Actually Look Like?
It’s not a one-and-done fix. Most patients start with monthly injections until the swelling goes down. Then, they switch to "as needed" - meaning they get checked every 4-8 weeks and get another shot only if swelling returns.
Real-world data shows patients need 8-12 injections in the first year to keep vision stable. Some need more. The average patient sees improvement by month 3-4. But if you miss appointments, vision can slip back.
Doctors use OCT scans to monitor progress. They measure the thickness of the macula - if it’s above 300 microns, treatment starts. When it drops below 250, they ease up. It’s science, not guesswork.
The injection itself takes about 5-7 minutes. Your eye is numbed with drops, cleaned with antiseptic, and held open with a tiny clamp. You might feel pressure, but not pain. A small amount of bleeding on the white of the eye is normal - it looks scary but clears up in days. Serious infections like endophthalmitis happen in less than 1 in 1,000 shots.
What Are the Downsides?
Cost is a huge barrier. Even with insurance, copays can hit $100-$200 per injection. For someone on a fixed income, 10 shots a year adds up fast. Some patients skip doses because they can’t afford it.
Then there’s the mental toll. The anxiety before each injection is real. One patient described it as "worse than the needle." The routine - clinic visits, waiting, the procedure - becomes exhausting. After 18 months, some people stop showing up, even when their vision is still improving.
Steroid implants like Ozurdex can cause cataracts in 60-70% of people who still have their natural lens. They also raise eye pressure in about 30% of cases, sometimes requiring drops or surgery. That’s why anti-VEGF is still the first choice for most.
And not everyone responds. About 20-30% of patients don’t gain much vision back, even with consistent treatment. That’s where new options are coming in.
What’s New in Treatment?
The future of RVO treatment is about fewer shots and smarter choices.
A new approach called "treat-and-extend" is gaining ground. Instead of monthly shots, you start with monthly injections, then slowly stretch the time between them - from 4 weeks to 6, then 8, then 12 - as long as your eye stays stable. A 2023 study showed this works just as well as monthly dosing but cuts injections by 30%.
There’s also new drugs in the pipeline. OPT-302, a drug that blocks a different growth factor, is being tested alongside Eylea. Early results suggest it helps patients who didn’t respond to anti-VEGF alone.
Gene therapy is on the horizon. RGX-314, currently in trials, aims to give your eye a long-term supply of anti-VEGF protein with just one injection. If it works, you might only need one shot every few years.
And then there’s Susvimo - a tiny pump implanted in the eye that slowly releases Lucentis. It’s already approved for another eye disease and is being tested for RVO. If it works here, monthly shots could become a thing of the past.
What Should You Do If You’re Diagnosed?
First, don’t panic. Vision loss from RVO isn’t always permanent. With treatment, 30-40% of patients reach 20/40 vision or better - enough to read, drive, and live independently.
Second, get your systemic health in check. See your GP. Control your blood pressure. Manage your diabetes. Lower your cholesterol. Quit smoking. These aren’t "nice to haves" - they’re part of your eye treatment plan.
Third, stick with the injections. It’s hard. It’s expensive. It’s tiring. But skipping doses risks permanent damage. Talk to your doctor about cost-saving options - Avastin is just as effective for many. Ask about financial assistance programs. Some clinics offer sliding scale fees.
Fourth, track your progress. Keep your OCT scans. Note when your vision changes. Bring your concerns to appointments. Your doctor needs to know if you’re struggling - not just with your eyes, but with your life.
Final Thoughts
Retinal vein occlusion is a serious condition, but it’s not a death sentence for your vision. Treatment has come a long way. What used to be a slow fade into blindness is now a manageable, often reversible, problem - if you act fast and stay consistent.
The key isn’t just the injection. It’s the follow-up. It’s the blood pressure check. It’s the commitment to show up, even when you’re tired. It’s knowing that your vision isn’t just about your eyes - it’s about your whole body.
Don’t wait for the next episode of blurred vision. If you’ve had sudden vision loss, even if it got better, get your eyes checked. You might be saving more than your sight - you might be saving your independence.
Can retinal vein occlusion be cured?
There’s no cure for the blocked vein itself, but the vision loss it causes can often be reversed or stabilized with treatment. Anti-VEGF and steroid injections reduce swelling in the macula, which is what blurs your vision. Many patients regain significant vision - up to 40% reach 20/40 or better. However, if treatment is delayed, permanent damage to the retina can occur, making full recovery impossible.
How many injections are needed for RVO?
Most patients start with monthly injections for 3-6 months until swelling clears. After that, treatment switches to "as needed," with check-ups every 4-8 weeks. On average, patients need 8-12 injections in the first year. Some need fewer with treat-and-extend protocols; others need more if the swelling returns. Long-term, many patients require 3-5 injections per year to maintain vision.
Are eye injections painful?
No, the injections themselves are not painful. The eye is numbed with anesthetic drops, and the needle is very fine. Most patients feel only slight pressure or a brief sting. The anxiety before the procedure is often worse than the actual shot. A small red spot on the white of the eye is common and harmless. Serious pain or vision loss after the injection is rare and should be reported immediately.
Can I drive after an eye injection?
You should not drive immediately after the injection. Your pupil will be dilated, and your vision may be blurry for a few hours. Most clinics recommend having someone drive you home. Avoid operating heavy machinery or reading fine print until your vision clears, which usually takes 2-4 hours. Don’t risk driving if you feel unsure - safety comes first.
What happens if I skip an injection?
Skipping an injection can cause fluid to build up again in the macula, leading to vision loss. Studies show that patients who miss appointments are more likely to lose vision long-term. Even if your vision feels fine, swelling can return without symptoms. Regular monitoring with OCT scans is essential. If you can’t make an appointment, call your clinic - they may be able to reschedule or suggest alternatives.
Can RVO happen in both eyes?
Yes, but it’s uncommon. Most people (about 85%) experience RVO in only one eye at first. However, over time, about 10-15% will develop it in the other eye, usually within 5 years. That’s why doctors monitor both eyes closely, even if only one is affected. Controlling risk factors like high blood pressure and cholesterol reduces the chance of it spreading.
Is there a link between RVO and stroke?
Yes. RVO and stroke share the same underlying causes - high blood pressure, atherosclerosis, diabetes, and blood clotting disorders. People with RVO have a slightly higher risk of stroke in the next 1-5 years. That’s why a diagnosis of RVO often triggers a full cardiovascular workup: blood tests, heart checks, and blood pressure monitoring. Treating your eyes means protecting your heart and brain too.
